Advanced Minimally Invasive HPB Surgery offers safer liver tumor treatment with faster recovery, lower risks, and improved patient outcomes. Advanced minimally invasive hepato-pancreato-biliary (HPB) surgery is changing how liver tumors are treated. Instead of large incisions, surgeons now use laparoscopic or robotic techniques that reduce trauma to the body. Patients often experience shorter hospital stays, quicker recovery, and lower complication rates compared to traditional open surgery.
Cost and recovery time are two of the most pressing concerns for anyone considering this option. The overall expense can vary depending on the hospital, technology used, and complexity of the tumor. Recovery usually takes weeks instead of months, with many patients returning to normal activities faster than after open liver surgery.

This article explores what advanced minimally invasive HPB surgery involves, who may benefit, how much it typically costs, and what recovery looks like. It also looks ahead at new techniques and technologies that continue to shape the future of liver cancer treatment.
Table of Contents
Overview of Advanced Minimally Invasive HPB Surgery
Advanced minimally invasive surgery for the liver focuses on reducing incision size, lowering complication risks, and improving recovery compared to traditional open methods. These procedures rely on specialized imaging, refined surgical tools, and expert training to safely address complex hepato-pancreato-biliary conditions.

Definition and Scope of HPB Surgery
Hepato-pancreato-biliary (HPB) surgery involves operations on the liver, pancreas, gallbladder, and bile ducts. These organs are closely linked in both function and anatomy, making surgical care in this region highly specialized.
Liver surgery often addresses tumors, both benign and malignant, as well as conditions such as bile duct blockages. Pancreatic and gallbladder procedures may target cancer, cysts, or gallstones.
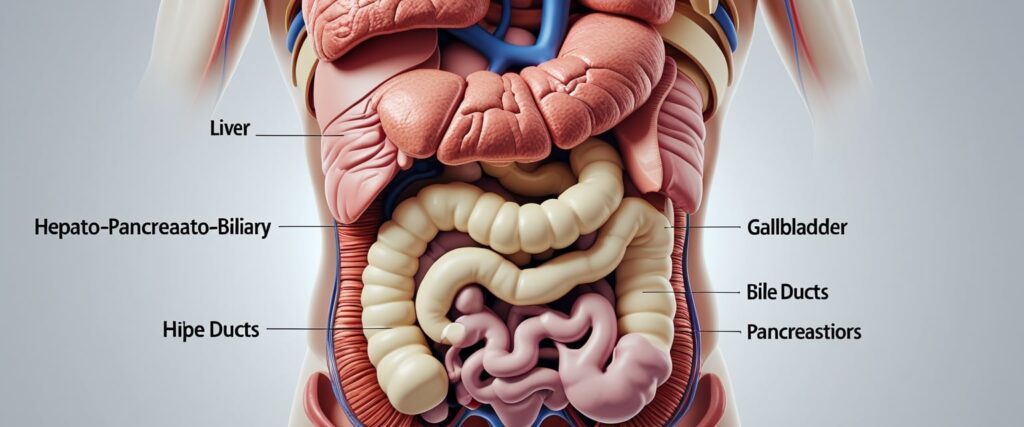
Minimally invasive HPB surgery uses laparoscopic or robotic techniques. Instead of a large incision, surgeons operate through small ports with cameras and instruments. This approach can treat a wide range of liver and biliary diseases that once required open surgery.
At leading centers like Johns Hopkins, HPB surgeons offer these advanced methods to manage both cancerous and non-cancerous conditions, often as part of a multidisciplinary care plan.
Evolution of Minimally Invasive Techniques
Minimally invasive HPB surgery has advanced rapidly in the last two decades. Early attempts were limited to small resections of the liver because of bleeding risks and technical challenges.
With improvements in laparoscopic cameras, energy devices, and stapling tools, surgeons can now perform complex resections with greater safety. High-resolution imaging and 3D visualization allow for precise planning and navigation during procedures.

Robotic systems add enhanced dexterity and control, expanding the range of operations that can be completed without open surgery. According to recent reviews, minimally invasive hepatobiliary surgery is now considered a standard option in many major centers.
Future developments may integrate artificial intelligence, virtual reality, and remote surgery technologies to further refine precision and safety in liver and biliary operations.
Key Differences from Open Liver Surgery
Open liver surgery requires a large abdominal incision, which increases recovery time, pain, and risk of complications such as hernias and infections. Minimally invasive techniques reduce these risks by limiting incision size.
Patients undergoing laparoscopic or robotic liver surgery often experience less blood loss, shorter hospital stays, and quicker return to daily activities. For example, laparoscopic liver surgery has been shown to lower the risk of abdominal hernias compared to open procedures.
The table below highlights some differences:
| Aspect | Open Liver Surgery | Minimally Invasive Surgery |
|---|---|---|
| Incision | Large (15–30 cm) | Small (0.5–2 cm ports) |
| Recovery time | Longer (weeks) | Shorter (days to 2 weeks) |
| Blood loss | Higher | Lower |
| Postoperative pain | Greater | Reduced |
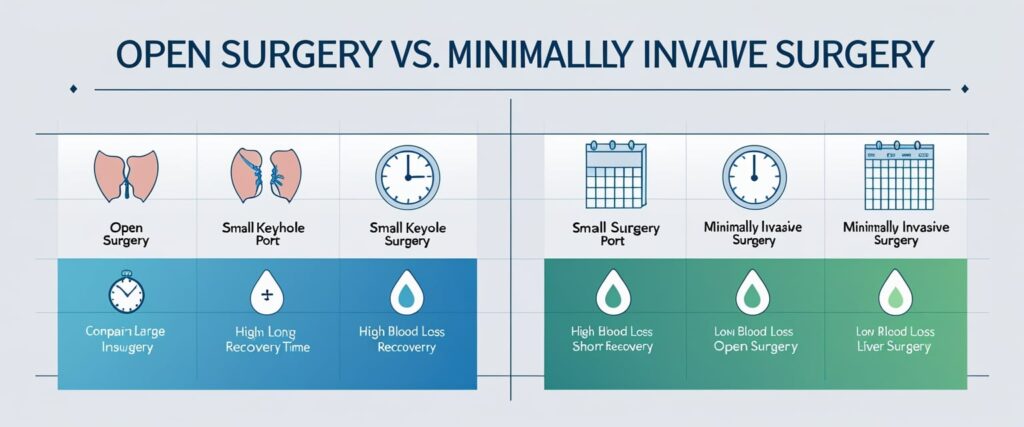
While not every patient is a candidate, minimally invasive HPB surgery offers significant benefits when performed by experienced surgical teams.
Types of Minimally Invasive Procedures for Liver Tumors
Minimally invasive liver surgery uses smaller incisions, advanced imaging, and precise surgical tools to remove or repair diseased tissue. These methods often reduce blood loss, shorten hospital stays, and lower complication risks compared to open operations.

Laparoscopic Liver Resection
Laparoscopic liver resection uses several small incisions and a camera to guide instruments. Surgeons can remove both benign and malignant tumors while preserving healthy liver tissue. This approach is especially effective for patients with localized disease and good liver function.
Compared to open surgery, laparoscopic liver surgery often results in less pain, shorter recovery, and fewer wound complications. Patients usually return to normal activities faster, though recovery still depends on the size and location of the resection.

Studies show that laparoscopic techniques can be safely applied to both primary and metastatic tumors. In experienced centers, outcomes are similar to open liver resection in terms of long-term cancer control, while offering the added benefit of reduced hospital stays. More details on these advances are described in minimally invasive surgical options for liver cancer.
Robotic HPB Surgery
Robotic HPB surgery uses robotic-assisted systems to perform complex procedures on the liver, pancreas, and bile ducts. The robotic platform provides enhanced visualization, greater dexterity, and more precise control than standard laparoscopy.
This approach is especially useful for tumors in difficult-to-reach areas of the liver. The robotic arms allow fine dissection around major vessels while reducing surgeon fatigue. As a result, robotic surgery is expanding in hepatobiliary cases that were once considered too challenging for minimally invasive methods.

Patients often benefit from smaller incisions, less blood loss, and faster recovery. While robotic surgery may involve higher upfront costs, it can reduce complications and hospital stays, which may offset expenses in some cases. A detailed review of these techniques is available in advances in minimally invasive liver surgery.
Cholecystectomy and Bile Duct Surgery
Cholecystectomy, or gallbladder removal, is one of the most common minimally invasive HPB procedures. It is often performed laparoscopically and serves as the foundation for more complex liver and bile duct operations.
For patients with cholangiocarcinoma or bile duct strictures, surgeons may perform minimally invasive bile duct resections and reconstructions. These procedures can involve removing part of the bile duct and reconnecting it to ensure proper bile flow.

Minimally invasive bile duct surgery remains technically demanding because of the delicate anatomy and risk of bile leakage. However, advances in laparoscopic and robotic methods have improved safety and outcomes. More information on these approaches can be found in current status of minimally invasive liver surgery for cancers.
Suitability and Patient Selection
Not every patient with liver tumors is an ideal candidate for minimally invasive surgery. Factors such as tumor size, location, overall liver function, and the patient’s health status strongly influence whether this approach is safe and effective. Careful planning by a specialized team helps reduce risks and improve recovery outcomes.
Criteria for Minimally Invasive Liver Surgery
Surgeons consider several criteria before recommending minimally invasive liver surgery. Tumor size is one of the most important factors. Small to medium tumors, typically less than 5–6 cm, are more suitable for laparoscopic or robotic approaches.
Liver function also plays a key role. Patients with healthy liver tissue or well-compensated cirrhosis may tolerate resection better than those with advanced liver disease. Blood tests and imaging studies help measure liver reserve and predict how much tissue can be safely removed.

Other important considerations include the patient’s age, body mass index, and surgical history. Prior abdominal operations can create scar tissue, which makes minimally invasive techniques more difficult. Patients with severe heart or lung conditions may also face higher risks and are often directed toward open surgery.
Tumor Types and Locations
The type and location of liver tumors strongly affect surgical planning. Primary liver cancer, such as hepatocellular carcinoma, is often treated with resection if the tumor is confined and liver function is preserved. Some cases of secondary tumors (metastases from colorectal cancer) are also good candidates for minimally invasive removal.
Tumors in the left lateral section of the liver are typically the easiest to remove using minimally invasive methods. This is because the anatomy is more accessible and less complex.

By contrast, tumors located near major blood vessels or deep within the liver present greater challenges. These cases may still require open surgery to ensure complete removal and reduce the risk of bleeding. Surgeons weigh these anatomical details carefully before making a recommendation.
Multidisciplinary Evaluation Process
Patient selection usually involves a multidisciplinary team that includes liver surgeons, oncologists, radiologists, and anesthesiologists. Each specialist contributes expertise to balance surgical risks with potential benefits.
Radiologists provide detailed imaging to map tumor size, number, and proximity to blood vessels. Oncologists assess whether surgery should be combined with chemotherapy or other treatments.

The team also evaluates recovery potential and long-term outcomes. For example, patients with widespread disease or poor liver function may be better served by nonsurgical options. This structured evaluation ensures that only patients most likely to benefit from minimally invasive liver surgery are selected.
Cost Factors in Advanced Minimally Invasive HPB Surgery
The cost of advanced minimally invasive HPB surgery depends on several measurable factors, including the method of surgery, the use of robotic systems, and the type of hospital where the procedure is performed. Patient expenses also vary depending on insurance coverage and the need for out-of-pocket payments.
Comparing Costs: Minimally Invasive vs Open Surgery
Minimally invasive surgery often requires higher upfront costs due to specialized tools and longer operating time. However, studies show that shorter hospital stays and fewer complications can offset these expenses. For example, increased use of minimally invasive techniques has been linked to reduced complication rates and significant national savings in hospital costs for common procedures (JAMA Network).
In HPB surgery, open operations may lead to longer recovery times and higher rates of infection or readmission. These complications increase both direct hospital charges and indirect costs, such as lost workdays.
A simple comparison:
| Factor | Minimally Invasive | Open Surgery |
|---|---|---|
| Average hospital stay | Shorter (by 1–3 days) | Longer |
| Complication risk | Lower | Higher |
| Upfront surgical cost | Higher | Lower |
| Long-term cost impact | Lower overall | Higher overall |

Influence of Technology and Hospital Facilities
Robotic surgery is common in advanced HPB procedures. Systems like the Da Vinci robot allow surgeons to perform complex liver resections with precision, but they increase costs due to high equipment prices and disposable instruments (Stanford Medicine).
Hospitals with established minimally invasive programs may reduce costs by spreading equipment expenses across a higher number of cases. In contrast, smaller hospitals may face higher per-case costs if they perform fewer procedures.

Facility resources also play a role. Access to advanced imaging, skilled surgical teams, and enhanced recovery programs can improve outcomes but add to the overall bill. Patients should understand that the choice of hospital can directly influence both cost and recovery experience.
Insurance and Out-of-Pocket Considerations
Insurance coverage often determines how much a patient pays for minimally invasive HPB surgery. Some plans cover robotic surgery at the same rate as traditional methods, while others may classify it as a higher-cost procedure.
Out-of-pocket costs depend on deductibles, copayments, and whether the hospital is in-network. Patients without full coverage may face higher bills for robotic-assisted operations, especially when specialized equipment is used.
It is important to ask about:
- Surgeon fees (may vary by experience in minimally invasive surgery)
- Hospital charges (facility fees, robotic system use, recovery room costs)
- Post-surgical care (follow-up visits, imaging, medications)

Clear communication with both the hospital billing office and the insurance provider helps patients avoid unexpected financial burdens.
Recovery Time and Postoperative Outcomes
Patients who undergo advanced minimally invasive HPB surgery for liver tumors often experience shorter hospital stays, reduced blood loss, and faster return to daily activities compared to open procedures. Careful follow-up and long-term monitoring remain essential to track healing, detect complications early, and support ongoing cancer care when needed.
Hospital Stay Duration
Minimally invasive liver surgery usually results in a shorter hospital stay compared to open surgery. Many patients are discharged within 3 to 5 days, while traditional open resections may require 7 to 10 days.
Smaller incisions and reduced trauma to surrounding tissues contribute to faster recovery. Patients also experience less postoperative pain, which allows earlier ambulation and quicker transition to oral diets.

Enhanced recovery protocols, such as early feeding and mobility, further shorten hospitalization. According to The Surgical Clinics, these approaches reduce discomfort and improve overall outcomes.
The length of stay can still vary depending on tumor size, complexity of the resection, and the patient’s overall health. Individuals with pre-existing conditions may need longer monitoring before safe discharge.
Return to Normal Activities
Patients often resume light activities within 2 to 3 weeks after minimally invasive HPB surgery. In contrast, recovery after open surgery may extend to 6 to 8 weeks.
Driving, walking, and returning to office-based work can usually occur earlier due to reduced pain and quicker wound healing. However, heavy lifting and strenuous exercise should be avoided for at least 4 to 6 weeks.

The use of smaller incisions decreases the risk of wound complications, which shortens recovery time. Stanford Medicine notes that minimally invasive approaches for liver and pancreas tumors lead to faster recovery and less discomfort.
Patients undergoing chemotherapy or additional treatments may need extended recovery before resuming all normal routines. Coordination with oncology teams ensures safe timing for restarting therapy.
Complications and Blood Loss
One of the major benefits of minimally invasive HPB surgery is reduced intraoperative blood loss. Smaller incisions and precise laparoscopic or robotic techniques help surgeons control bleeding more effectively than in open surgery.
Lower blood loss reduces the need for transfusions, which decreases the risk of infection and speeds recovery. A review in ScienceDirect highlights that minimally invasive approaches consistently report less blood loss and shorter recovery times.

Complication rates, such as infection or bile leaks, are generally similar or slightly lower compared to open procedures. The reduced trauma from minimally invasive techniques also lowers the risk of wound infections.
Still, complex resections involving multiple tumors or fragile liver tissue can increase complication risks regardless of the surgical approach. Careful patient selection remains important.
Follow-Up Care and Long-Term Monitoring
After discharge, patients require structured follow-up care to ensure proper healing and to monitor for recurrence of liver tumors. Typical care includes wound checks, liver function tests, and imaging studies such as CT or MRI scans.
Follow-up visits usually occur within 1 to 2 weeks after surgery, then at regular intervals every few months depending on the diagnosis. Patients treated for cancer often need closer surveillance to coordinate with chemotherapy or targeted therapies.

According to Johns Hopkins Medicine, specialized HPB teams provide long-term monitoring to track both recovery and cancer outcomes.
Patients are also advised on lifestyle adjustments, including nutrition and physical activity, to support liver health. Long-term engagement with the surgical and oncology team helps detect complications early and maintain quality of life.
Future Directions and Innovations in Minimally Invasive HPB Surgery
Advances in surgical technology and clinical practice continue to reshape how hepatobiliary and pancreatic (HPB) procedures are performed. These changes focus on improving precision, lowering complication rates, and making complex surgeries more widely accessible.
Technological Advancements
Robotic surgery is becoming a central tool in HPB operations. Compared with traditional laparoscopy, robotic systems provide 3D visualization, enhanced dexterity, and tremor reduction. These features allow surgeons to perform delicate tasks, such as bile duct reconstruction, with greater accuracy. Institutions worldwide are reporting steady growth in robotic HPB procedures, reflecting improved safety and feasibility.
Integration of artificial intelligence (AI) and imaging technologies is another key step. AI can assist with intraoperative navigation, margin detection, and decision support. Virtual and augmented reality tools also help in preoperative planning, allowing surgeons to map out tumor resections in detail.

Future platforms may combine robotics, AI, and real-time imaging into a single operating system. This could shorten operative times and improve outcomes in complex liver tumor resections. Research highlights that minimally invasive surgery is moving toward becoming more intelligent, compact, and multifunctional, as described in current reviews of minimally invasive hepatobiliary surgery.
Expanding Indications for Minimally Invasive Approaches
Minimally invasive techniques are now applied to a wider range of liver tumors. While early adoption focused on small, superficial lesions, surgeons are increasingly performing resections for larger or centrally located tumors. This includes hepatocellular carcinoma, colorectal liver metastases, and selected cases of cholangiocarcinoma.
Robotic surgery has been especially useful in expanding these indications. Its precision allows surgeons to operate in tight spaces and perform complex reconstructions. Studies show that with growing expertise, procedures once limited to open surgery can now be performed laparoscopically or robotically in high-volume centers.

Living donor liver transplantation and two-stage hepatectomy are also areas where minimally invasive approaches are being explored. Reports from specialized programs suggest these methods can be safe when performed by experienced teams, as noted in reviews of advances in minimally invasive liver surgery.
As training improves and technology spreads, more patients with liver tumors may become candidates for minimally invasive HPB surgery, reducing recovery time without compromising oncologic outcomes.
Conclusion
Advanced minimally invasive HPB surgery offers liver tumor patients safer procedures, faster recovery, and reduced complications compared to open surgery. While costs may vary, the long-term benefits in comfort, recovery, and outcomes make it a promising option for many patients.
Frequently Asked Questions
Advanced minimally invasive HPB surgery for liver tumors often involves higher upfront costs but may reduce hospital stays and speed up recovery. Outcomes depend on tumor type, patient health, and surgical approach, with robotic and laparoscopic methods offering different advantages and challenges.
What is the average cost of advanced minimally invasive surgery for liver tumors?
The cost of minimally invasive liver surgery can vary widely. Factors include hospital location, surgeon expertise, and use of robotic systems. Some studies note that laparoscopic procedures may lead to higher charges due to longer operative times and specialized instruments, though shorter hospital stays can offset expenses (Enhanced Recovery After Surgery: Hepatobiliary).
How long is the recovery period following minimally invasive HPB surgery?
Patients often experience shorter recovery times compared to open surgery. Hospital stays can be reduced by several days, and many return to normal activities within a few weeks. Recovery speed depends on the extent of resection, overall health, and whether the surgery involved bile duct reconstruction.
What are the benefits of choosing minimally invasive surgery over traditional open surgery for HPB procedures?
Minimally invasive techniques usually result in less blood loss, smaller incisions, and faster recovery. Patients often report less discomfort and a quicker return to daily life. Institutions such as Stanford Medicine highlight reduced pain and shorter hospital stays compared to open procedures.
Are there any potential risks or complications associated with minimally invasive liver surgery?
Risks include bleeding, infection, and bile leakage. In some cases, patients with fragile or diseased livers may face higher complication rates. Surgeons also note that complex reconstructions, such as bile duct or vascular repairs, carry added technical challenges (Current status of minimally invasive liver surgery).
What factors can influence the cost and recovery time for HPB surgery?
Key factors include tumor size, number of tumors, liver function, and prior treatments. The use of robotic systems may increase costs, while enhanced recovery programs can shorten hospital stays. Patient age, pre-existing conditions, and need for additional procedures also play a role in both expense and recovery.
How effective is minimally invasive HPB surgery in treating liver tumors compared to other treatments?
Minimally invasive liver surgery shows outcomes comparable to open surgery for many patients. Studies report similar long-term survival rates when performed in specialized centers. For select cases, robotic and laparoscopic methods may improve precision and reduce surgical stress, making them valuable options for both primary and metastatic liver tumors.
